Temperature Assessment via the Temporal Artery
What Exactly is Being Measured?
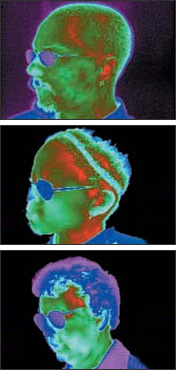
It is helpful to see exactly what we are targeting when we are measuring temperature with the Temporal Artery Thermometer, and the following images will illustrate the areas of interest.
It is not uncommon to see someone scanning down the side of the face, following the curve of the eyebrow. As you can see from the thermal images, a scan down the side of the face is apt to miss the temporal artery altogether as the temporal artery can go fairly deep in that area, varying from individual to individual.
Scanning down the side of the face also results in non-reproducibility of the reading, whereas, scanning straight across the temporal artery is reproducible within, allowing approximately 30 seconds between scans so as to let the skin recover from the cooler probe of the thermometer.
Learn more:
TemporalScanner™ Temporal Artery Thermometry

With just a light stroke across the temporal artery area of the forehead, an accurate reproducible temperature is measured in about 3 seconds – eliminating any discomfort caused by a thermometer inserted into the ear, mouth, or rectum. Designed specifically to be completely non-invasive, the TemporalScanner is a most significant advance, applying Exergen’s well-proven Arterial Heat Balance (AHB) technology to the most convenient site possible.
Branching from the external carotid, the superficial temporal artery courses about 1 mm below the skin of the lateral forehead, providing good heat conduction to the skin surface. The TA is readily accessible, and provides no risk of injury from being touched. Since it is not an anastomosing vessel, perfusion remains high and stable, ensuring the reliability of conditions for the patented AHB method to compute accurate temperatures. High resolution infrared images confirm the reliability of the heat signature of the TA area for all ages.
Arterial Heat Balance (AHB) at the Temporal Artery at Room Temperature
Blood at Ta Is supplied to the temporal artery from the aorta via the carotids, and is cooled by heat energy lost to the environment at te resulting in cooler Tta, By measuring this heat loss and adding it back to Tta the AHB is formed and Ta is then recovered.
Measure straight across the forehead – you’ll never miss the temporal artery.
Use Cases
A Morbidly Obese Patient
For reference, the black circles are eyeglasses, the orange “Y” is the temporal artery. Measure straight across the forehead and you’ll never miss the temporal artery even on a morbidly obese or edematous patient. Note how the artery is lost on the side of the face just above the stem of this patient’s glasses. Note how curving down at the eyebrow would miss the artery altogether.
Head Trauma and Bandages
Interestingly, if the image above were one of a head trauma patient (whether from a surgeon’s scalpel or a vehicle), the physical properties exhibited in the above image will be present because vasodilation is assured (Mother Nature immediately rushes blood to the area of trauma in order to begin the healing process). And, although the temporal artery area might be completely covered with bandages, since vasodilation is assured, we could make the measurement with just a short scan on the neck.
Normal Perfusion

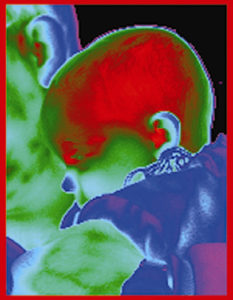
A common question we are frequently asked is why we don’t just measure temperature on the neck rather than at both forehead and neck.
The problem with just using the neck is clearly illustrated by the image on the left. This patient is not sweating, not dumping heat, and appears to be quite comfortable, at least according to her perfusion pattern.
Nonetheless, this patient’s neck is as cool as a clam, and measuring temperature on her neck, but not across the temporal artery, would result in a falsely low temperature.
It is important to note that vasodilation can only be assured (without using a Doppler) if the patient is diaphoretic, or has suffered head trauma.
Burn Patients
Interestingly, a burn patient exhibits a continuous state of vasodilation as does an infant. A burn patient is also cared for in a warm environment, and requires a high caloric intake to make up for the heat that is continually being lost to the environment. Accordingly, the same temperature measurement technique as with infant applies.
Should there be no intact skin, the temperature can still be accurately taken at the temporal artery area by applying a film strip** over the temporal artery area. The film becomes an impermeable barrier to moisture, and therefore prevents any effect from evaporative cooling of the tissue. This allows a scan to be made on top of the film strip, without the requirement to scan on the neck area behind the ear. And, the strip will self-adhere as long as the tissue is moist.
** The film strips are available in a carton of 10 little boxes, each containing a roll of 250 film strips, Exergen part number 128800, available from hospital’s preferred suppliers or from Exergen.

Diaphoresis
This image illustrates how the effect of evaporative cooling on the forehead of a sweaty patient would erroneously lower the temperature.
The one critical requirement for measuring arterial temperature is vasodilation. The temporal artery has no appreciable vasomotor activity, and as such, maintains a nearly constant rate of perfusion.
Note the redness of the neck in the image to the left, which is indicative of vasodilation. And, since we sweat first on the forehead area, we sweat LAST on the neck area, making it an excellent area on which to use the temporal artery thermometer.
By measuring both the area over the temporal artery, and the area behind the ear on the neck, the temporal artery thermometer will capture the highest of 3,000 uptakes, selecting the highest pinpoint of heat it sees. If the forehead is wet, the neck will override, and if the forehead is dry, the measurement on the neck is a throwaway, but eliminates discretion, and allows for uniformity in the measurement as everyone is standardized on the technique.
If the patient is completely soaking wet, you cannot wipe the sweat away quick enough to have any effect on the measurement. At this point, the patient’s temperature is dropping rapidly, fever is not an issue, and the best procedure would be to return in about 10 minutes to take a temporal artery temperature when the patient should be dry.
If you have a diaphoretic patient whose temperature needs to be taken STAT, or are treating a patient with hyperhydrosis, please see the information on using a film strip at the bottom of this page.
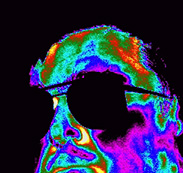
An Infant is a Little Radiator
Infants are analogous to little radiators. The infant on the left is being held by his father, and just came in from the freezing cold outdoors. The little blue circle just left of center is his cold little nose. But, just look at the color of his head. The red indicates the heat being released from the blood vessels which are constantly dilated, even in the extreme cold. This is because vasomotor control does not mature until they are around 11 months old. The fact that we strive to maintain a warm environment for an infant, either by swaddling or by use of an isolette or radiant warmer, bears witness to this analogy.
This constant state of vasodilation allows a temporal artery temperature to be taken just by a gentle touch to the temporal artery area (easier to depress the button prior to touching an infant’s head), or by a 2 inch microscan across the temporal artery area.





